In 2016, the World Health Organization (WHO) announced that since 2000, average global lifespans had extended by a full five years – the fastest rise since the 1960s. While there remain tremendous variation by country, and inequality within countries across different gender, ethnic, and socio-economic groups, people across the globe are generally living longer. But underlying this good news is a knotty policy challenge. Healthy life expectancies or healthspans – the number of years one can expect to live in good health – are extending at a markedly slower pace in most countries. This growing gap fuels fiscal concerns and policy debates over rising costs – how can societies best meet the healthcare and long-term care needs of today’s older adults, and improve the health outcomes of future generations? Three consistent patterns regarding older adult care are emerging across countries, including: a shift toward home- and community-care to support aging in place; a sweeping focus on promoting healthy lifestyles in future generations, and growing interest in leveraging digital technology to improve access and the efficiency and quality of care.
The global population age 80 or older will more than double to reach 4.3 percent by 2050. The largest percentage will be in Japan, where every two in five older people will be age 80 or older.
Healthcare System
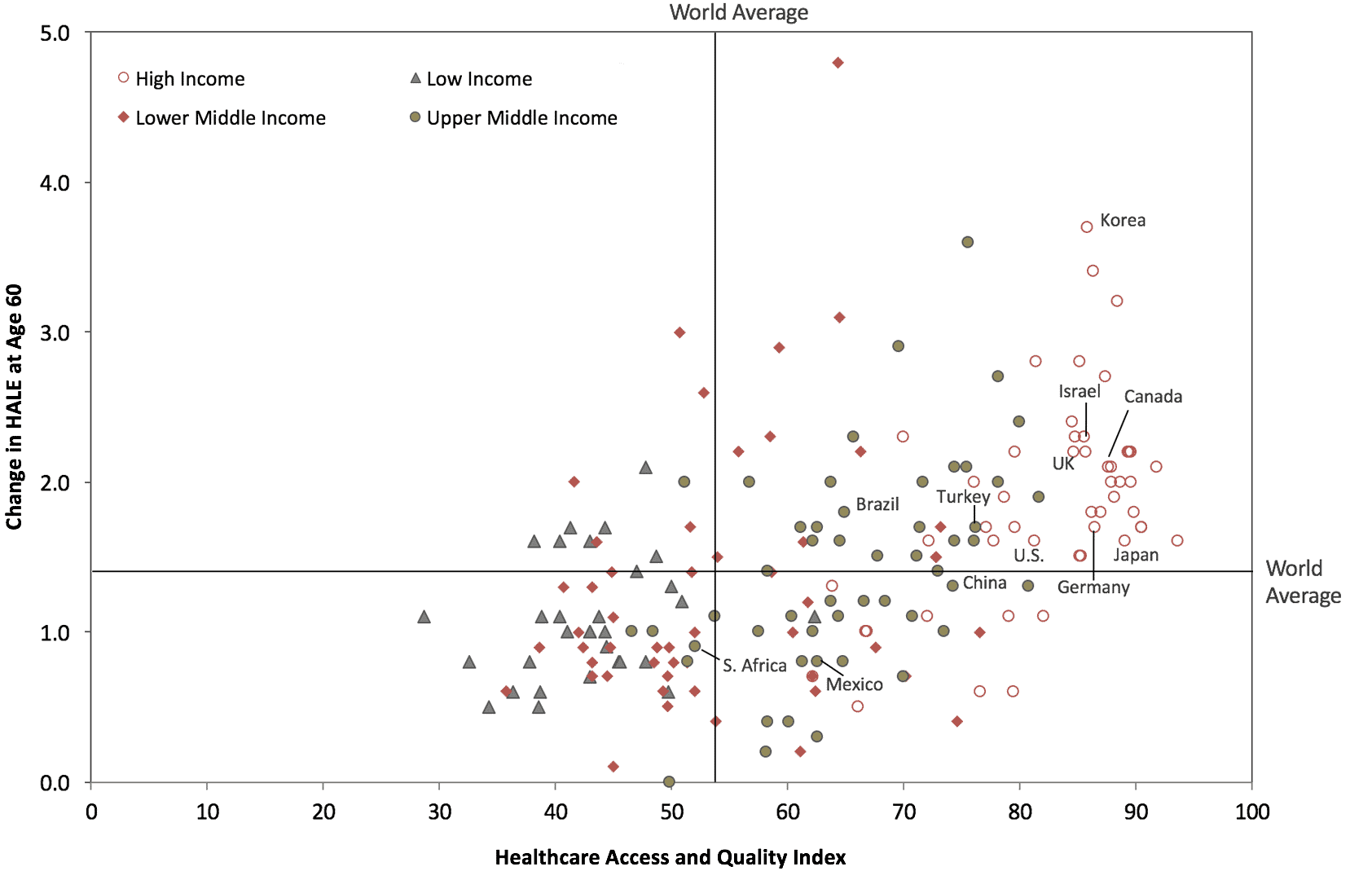
Coupled with the widening gap between lifespans and healthspans is a significant divergence in older-age health across countries. Uneven access to and quality of healthcare are among the contributing factors. Universal healthcare coverage is crucial to addressing the healthcare challenges facing older adults. Although UN Member States agreed to work toward UHC by 2030 as part of the Sustainable Development Goals, growing fiscal concerns challenge their commitment. The most remarkable progress has been seen in emerging market countries, with a focus on providing financial protection and expanding access to preventive and primary care. Around the world, information and communication technology could play a pivotal role in promoting universal health coverage. With rapid expansion in the adoption of digital technology – particularly mobile devices – and substantial advancement in areas like sensors and cloud computing, eHealth promises to become an essential component of the health system.
Each year, 100 million people around the world are pushed into poverty, and 150 million suffer financial catastrophe because of out-of-pocket healthcare expenditures, and the older population is among the most vulnerable. Yet one in four countries does not have a national policy or strategy for universal healthcare.
Between 1990 and 2015, at least 73 countries adopted eHealth policies or strategies, with nearly two-thirds of the adoption occurring in the last five years. More than 90 percent of these policies and strategies include objectives that address how eHealth can contribute to universal healthcare. However, a lack of funding and infrastructure are among the biggest barriers to promoting eHealth.
Change in Healthy Life Expectancy at Age 60 (2000-2015) vs. Healthcare Access and Quality Index in 2015
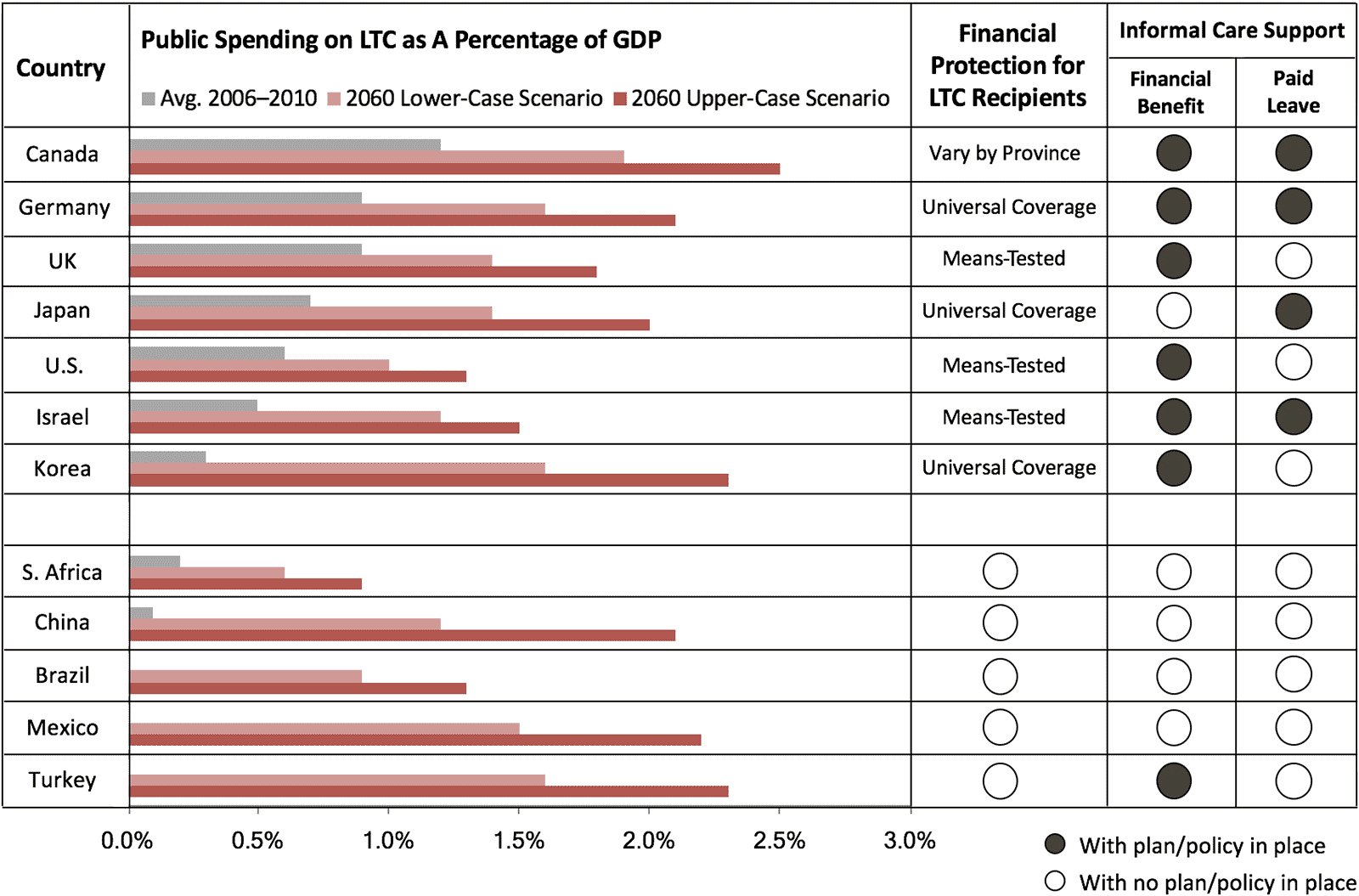
Long-Term Care
Unlike healthcare, which governments often deem to be a core component of social policy, long-term care (LTC) receives much less public attention and spending, and the provision of LTC varies widely. LTC generally refers to the care of people with or at risk of a significant and ongoing loss of physical capacity to function in their daily activities, both at home and within dedicated facilities. While a looming fiscal challenge, there are models emerging around the world for cost-effective LTC, with an increasing focus on supporting aging in place. Early progress is also being made in countries that are already grappling with a shrinking labor force and a rising dementia crisis, providing valuable experience for the rest of the world.
Turkey’s Caregiver Service Program
Turkey introduced the Caregiver Service Program in 2007 to subsidize caregiving for low-income older adults and their families. The program was designed to compensate family members for the financial loss associated with leaving a job to care for an older relative and to create an incentive for women to enter the labor force as external caregivers. Family members or external caregivers dedicating at least eight hours per day to caregiving receive a monthly wage. Those with incomes no higher than two-thirds of the minimum wage are eligible for external caregivers, and in families living at this limited income level, relatives can receive the subsidy. The monthly wage/subsidy is subject to adjustment every six months and stood at TRY 881 (approximately USD 280) as of the second half of 2016, or just over half of the minimum wage. Even though the subsidy is only half of the minimum wage, it is believed by experts to be an incentive for caregivers, who are usually women not active in labor force, hence helping to both increase women’s labor participation and improve care for the aging population.
Life-Course Health Promotion
While access to healthcare and long-term care is crucial for today’s older people, health promotion across the entire population benefits future generations and facilitates the sustainability of health and LTC systems in an era of rapid aging. Promoting healthy lifestyles is a proactive, cost-effective approach to address the spread of noncommunicable diseases, a growing major health threat around the world. Government action is on the rise in this area, although significant variability suggests that more work needs to be done.
Globally, the prevalence of NCDs among the population ages 15 through 64 is increasing – between 1990 and 2015, this group saw the NCD-related disease burden rise by 54 percent. Obesity is a leading factor in the growing risk of NCDs. Its occurrence has more than doubled globally since 1980.
Ninety-three percent of 160 countries responding to a 2015 WHO survey reported to have established a unit or department in the Ministry of Health responsible for NCDs, up from 88 percent five years ago, but this varies significantly by region and focus area.
Germany Strengthens Health Promotion
The most successful models for promoting healthy lifestyles combine a top-down policy push with specific goals and measures, dedicated budgets, and promotion of cross-sector collaboration. Germany stands out with enactment of the Act to Strengthen Health Promotion and Preventive Healthcare in 2015. The law requires the allocation of half a billion euros – a nearly 75 percent increase from the previous budget – from health insurance and nursing funds each year. At least three-fifths of the budget will be used in health promotion within schools, municipalities, workplaces, and nursing homes, including diet, exercise, stress reduction, and addiction prevention. To ensure effective implementation, the law also emphasizes collaboration across government actors and on federal and local levels to identify joint goals and approaches.
Key Takeaways
Meeting the healthcare and wellness needs of today’s older adults and working to promote healthy lifestyles in younger generations are twin challenges that require an immediate, redoubled commitment from governments around the world. As in other areas of aging policy, fiscal constraints threaten to force short-term, siloed approaches that produce larger costs and threaten the long-term competitiveness and prosperity of societies. While no country has cracked the code for healthy aging, it is clear that there are manifold opportunities to achieve greater efficiency and improved well-being:
- Promotion of preventive care and a healthy lifestyle is a proactive, cost-efficient solution to close the gap between lifespans and healthspans across generations.
- Supporting caregiving, by ensuring the flexibility to allow family members to provide short-term care while remaining active in the labor market, and creating incentives to increase the formal caregiving labor force will both be vital to accommodate rising demand for LTC outside of costly institutional settings.
- Technology, such as eHealth and robotics, promises to be an integral element of health and long-term care. It offers an opportunity to expand access and lower costs, as well as drive economic growth and competitiveness for those countries and companies that effectively seize it.